Living with vitiligo can be stressful. Between 0.5% and 2% of people worldwide experience this condition, and the sudden appearance of white patches on the skin can affect confidence and daily life. We understand how unsettling it can be to notice these changes and worry about how the condition may progress.
Evidence-based vitiligo treatment offers options to slow the spread of depigmentation, support re-pigmentation, and help patients feel more in control of their skin health. It’s not just about restoring colour; it’s about giving you practical steps, guidance, and reassurance throughout the journey.
This blog explains how vitiligo is diagnosed, the treatment options available, and daily care strategies that support both skin and confidence. Understanding these aspects can help patients and families make informed choices and feel supported every step of the way.
Overview
- Vitiligo occurs when the immune system attacks pigment cells, causing white patches on the skin that can affect confidence and daily life.
- Early diagnosis through medical history, skin exams, Wood’s lamp, and lab tests improves treatment effectiveness and slows progression.
- Treatment combines medicine, light therapy, and, in some cases, surgical options to encourage repigmentation and prevent new patches.
- Daily care, sun protection, stress management, and a balanced diet support skin health and enhance treatment results.
- Emotional and social support from professionals, peer groups, and family strengthens coping and improves overall outcomes.
What is Vitiligo?
Vitiligo is a skin condition in which the immune system attacks melanocytes, the cells responsible for producing skin pigment. This immune response damages melanocytes, leading to the appearance of white patches on the skin.
It affects people of all genders equally, with men and women developing the condition at similar rates. Vitiligo is a widely seen skin concern across different populations.
The white patches often appear in a symmetrical pattern on both sides of the body. They can develop anywhere but are most common in areas exposed to the sun, friction, or injury. Early detection and proper medical evaluation help ensure the most effective vitiligo treatment approach.
Causes and Risk Factors of Vitiligo

Vitiligo can happen due to a combination of genetic factors, immune system changes, and specific environmental triggers. Knowing these possible causes can help in understanding the condition and planning the most effective vitiligo treatment.
The condition develops due to several factors working together, which is why it can appear differently in each person and respond in varied ways to treatment.
Possible Causes of Vitiligo
The primary causes behind vitiligo development include several interconnected mechanisms:
- Autoimmune response: In some people, the immune system wrongly identifies pigment-producing cells (melanocytes) as harmful and destroys them.
- Oxidative stress: An excess of unstable molecules called free radicals can damage melanocytes, triggering skin pigment loss.
- Genetic changes: Certain inherited traits may make melanocytes more fragile or prone to immune attack, increasing the risk of vitiligo.
- Cell connection issues: Weak attachment between melanocytes and surrounding skin tissue can cause these cells to break away and die.
- Ongoing inflammation: Chronic inflammation in the skin can repeatedly damage melanocytes, leading to the gradual spread of white patches.
- Metabolic changes: Disruptions in how melanocytes use energy and nutrients can make them less able to survive everyday stressors.
Risk Factors for Vitiligo
Some people are more likely to develop these skin conditions due to the following factors:
- Family history: Having a parent, sibling, or close relative with vitiligo can increase the chances of developing the condition.
- Age: Vitiligo can occur at any age, but it often appears before the age of 30. Early onset may be linked to faster progression.
- Other autoimmune conditions: People with conditions like thyroid disease, type 1 diabetes, rheumatoid arthritis, or alopecia areata have a higher risk.
- Thyroid disorders: Vitiligo is often associated with thyroid problems, especially hypothyroidism, making regular thyroid checks essential.
- Skin injury or friction: Cuts, burns, or repeated rubbing of the skin can sometimes trigger new patches in vulnerable individuals. This is known as the Koebner response.
- Chemical exposure: Contact with certain industrial chemicals, some hair dyes, or harsh cosmetic products may trigger vitiligo in predisposed people.
- High stress levels: Significant emotional stress or traumatic events may play a role in the onset or worsening of vitiligo.
- Severe sunburns: Intense sunburn, especially during childhood, can increase the risk in those already prone to the condition.
Common Symptoms and Types of Vitiligo

Spotting vitiligo early can help with timely diagnosis and treatment planning. The condition has clear signs that a dermatologist can confirm during an examination. Its appearance and speed of progression vary; some people notice quick changes, while others see slow, gradual changes over many years.
Symptoms to Watch For
- White or pale patches on the skin where pigment is lost.
- Hair in affected areas is turning white or grey, including eyebrows and eyelashes.
- Loss of colour inside the mouth or nose.
- Changes in eye colour, including the retina.
- Patches are becoming more noticeable after sun exposure.
- Depigmentation appears in a similar pattern on both sides of the body.
The way vitiligo appears can also depend on its type. Understanding these types can help patients and doctors choose the most suitable treatment approach.
Types of Vitiligo
- Generalised vitiligo: The most common form, with patches appearing on several parts of the body in a symmetrical pattern
- Segmental vitiligo: It affects only one side or a specific section of the body, often in younger individuals.
- Focal vitiligo: Limited to one or a few small areas, with no clear spread
- Universal vitiligo: Extensive pigment loss covering most of the skin
- Acrofacial vitiligo: Appears on fingers, toes, and areas around the mouth, eyes, and other body openings.
- Mucosal vitiligo: Affects the lining inside the mouth or the genital area.
How is Vitiligo Diagnosed?
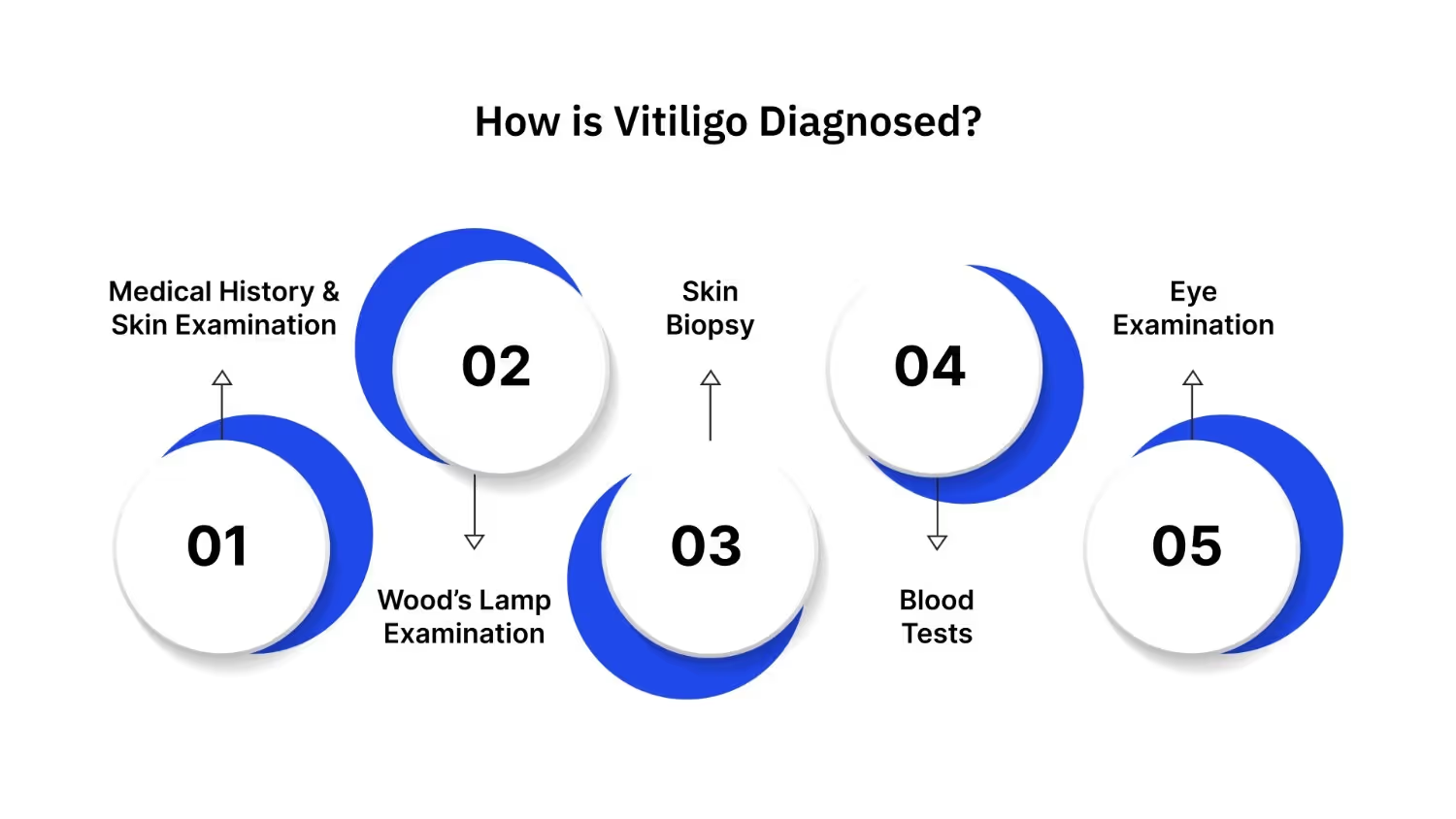
Getting an accurate diagnosis is the first step in planning effective vitiligo treatment. Dermatologists use several methods to confirm vitiligo and rule out other skin conditions with similar symptoms. The earlier the diagnosis, the better the chances of slowing progression and reducing uncertainty.
1. Medical History and Skin Examination
Diagnosis usually starts with a conversation and a close look at your skin. This helps your dermatologist understand your health background and spot visible signs of vitiligo.
What this involves:
- Questions about family history of vitiligo or autoimmune diseases.
- Discussion of recent illnesses, stress, or medications.
- Visual check of the size, shape, and location of light patches.
- Assessment of whether patches are symmetrical on both sides of the body.
2. Wood’s Lamp Examination
If the patches are subtle, the dermatologist may use a Wood’s Lamp, a special ultraviolet (UV) light, to see them more clearly.
What this involves:
- The light shines over the skin in a darkened room.
- Vitiligo patches appear with sharp contrast against normal skin.
- Helps detect early or faint patches that may not be visible under standard lighting.
3. Skin Biopsy
When visual signs are unclear, a skin biopsy can provide a definite answer. This involves taking a small sample of skin for lab testing.
What this involves:
- Local anaesthesia is applied to numb the area.
- A small piece of skin is removed using a shave or punch tool.
- The sample is examined under a microscope to check for missing melanocytes.
4. Blood Tests
Because vitiligo can be linked to autoimmune disorders, doctors often check for other underlying conditions.
What this involves:
- Thyroid function tests to detect hypothyroidism or hyperthyroidism.
- Vitamin B12 level check.
- Antibody tests to look for other autoimmune activity.
5. Eye Examination
In some cases, vitiligo may also affect parts of the eye, particularly the retina. An eye exam can catch these changes early.
What this involves:
- Your medical help can use specialised equipment to examine the retina and other structures.
- Checks for pigment loss or inflammation inside the eye.
- Helps prevent potential vision complications with early treatment.
If you notice any new or changing patches, schedule a call with Dr. Janani Sree C M at Velantis Dermatology. Early assessment ensures accurate diagnosis and the most effective vitiligo treatment plan.
Goals of Vitiligo Treatment

Effective vitiligo treatment aims for practical, measurable results that improve a patient’s quality of life. A clear understanding of these goals helps set realistic expectations and track progress. Modern approaches often combine therapies to address different aspects of the condition at the same time.
Outcomes vary significantly between individuals. Factors such as the location, size, and duration of patches, as well as the patient’s age, can influence how well treatment works. Involving an experienced dermatologist ensures that the most suitable methods are chosen for each case.
Key treatment goals include:
- Slowing or stopping the spread of new patches.
- Encouraging re-pigmentation in existing affected areas.
- Preventing recurrence in treated regions.
- Supporting emotional well-being and improving overall quality of life.
- Managing associated autoimmune conditions effectively.
While some areas respond more positively to treatment, others may remain resistant. For example, facial and neck patches often show faster and more noticeable improvement compared to patches on the hands or feet. Maintaining realistic expectations helps patients stay motivated throughout the treatment process.
Medical and Procedural Vitiligo Treatment Options
Vitiligo can be treated in several ways, and the choice of treatment often depends on factors such as the size and location of patches, the patient’s age, and whether the condition is still spreading. In many cases, using a combination of treatments works better than relying on one method alone. This can help improve colour return (re-pigmentation) and slow down or stop the appearance of new patches.
Pharmacological (Medicine-Based) Treatments
Doctors may recommend creams, ointments, or tablets to control vitiligo and encourage pigment cells to return. Common options include:
- Corticosteroids – Often the first choice, these anti-inflammatory medicines help calm the immune system so it stops attacking pigment cells (melanocytes). Creams work best on areas like the face and neck, and can bring good colour return if started early.
- Calcineurin inhibitors – Medicines like tacrolimus and pimecrolimus are valuable alternatives to steroids, especially for delicate skin such as the face and eyelids. They reduce immune activity without some of the long-term side effects of steroids.
- JAK inhibitors – A newer development in vitiligo care. Ruxolitinib cream is the first approved JAK inhibitor for vitiligo. It blocks specific pathways that cause melanocyte damage.
- Vitamin D analogues – These help balance immune activity and may support melanocyte survival. They are often used alongside other treatments.
While medicines can control immune activity and protect pigment cells, they work best when combined with light-based treatments that stimulate pigment production.
Light-Based Therapies
Light therapy is a key part of vitiligo management, as certain types of UV light can activate melanocytes and encourage pigment return. Options include:
- Narrowband UVB phototherapy – Considered one of the most effective treatments. It uses a safe wavelength of UV light to stimulate pigment cells, usually given two or three times per week in a clinic.
- Excimer laser – A focused form of UVB light, ideal for treating small patches. It targets only the affected area, reducing unnecessary exposure for healthy skin.
- PUVA therapy – Combines a medicine called psoralen with UVA light. It can help in widespread vitiligo, but is used less often now because of possible side effects.
- Depigmentation therapy – For people with vitiligo affecting over 80% of the skin, removing the remaining pigment can create a more even skin tone. This is usually considered a last-resort option.
If vitiligo patches have been stable for some time and haven’t responded to medical or light treatments, surgery may be an option.
Surgical Treatment Options
Surgical treatments aim to move pigment-producing cells from healthy skin to affected areas. They are usually only recommended when vitiligo has been stable for at least 6–12 months.
- Skin grafting – Small sections of normal skin are transplanted onto vitiligo patches. Works best for small, stable areas.
- Blister grafting – Suction is used to create small blisters on healthy skin. The top layer (with pigment cells) is then placed over depigmented patches.
- Non-cultured epidermal suspension – Pigment cells are collected from a small sample of healthy skin, processed, and then applied to the affected area. This method can treat both small and large patches with good results.
Starting a vitiligo treatment plan under professional care can make a real difference. At Velantis Dermatology, Dr. Janani Sree C M helps patients find the right combination of therapies and support to suit their skin and lifestyle. Book a call to start your healing journey.
Self-Care and Daily Management
Daily self-care is not just about protecting the skin; it is about feeling more in control during the vitiligo treatment journey. While medical treatments address the condition directly, these everyday steps can protect sensitive skin, reduce triggers, and support emotional well-being. They also help minimise discomfort and prevent complications, though they work best when combined with professional care.
Practical steps that can make a difference
- Apply a broad-spectrum sunscreen (SPF 30 or higher) every day to protect depigmented areas from sunburn and further pigment loss.
- Wear hats, scarves, or long sleeves during outdoor activities to shield the skin from UV exposure.
- Avoid contact with harsh chemicals or skin irritants that could cause new patches or worsen existing ones.
- Manage stress through relaxation techniques, gentle exercise, or counselling, as emotional strain can influence skin health.
- Eat a balanced diet rich in antioxidants and essential nutrients to support immune function.
- Choose loose-fitting, breathable clothing to prevent friction and irritation on affected areas.
- Use gentle, fragrance-free skincare products that keep the skin moisturised without causing reactions.
- Stay hydrated and ensure adequate sleep to help the body repair and maintain resilience.
Camouflage makeup can also provide a confidence boost during treatment. A dermatologist or skincare specialist can guide you in choosing products that are safe for sensitive skin and compatible with ongoing therapies.
How to Support Yourself While Managing Vitiligo?
Caring for vitiligo goes beyond treating the skin. Protecting emotional well-being is just as important, and there are practical steps that can make this journey easier.
- Seek professional help when needed: A qualified mental health professional can guide you through anxiety, stress, or low mood, helping you build healthy coping skills.
- Join a support group: Connecting with others who truly understand your challenges can reduce feelings of isolation and create a safe space to share experiences.
- Learn more about your condition: Understanding vitiligo helps you address misconceptions with confidence and reduces the fear of the unknown.
- Involve your family: Share information with your loved ones so they can provide the proper support and encouragement at home.
- Practice stress management: Activities like meditation, gentle yoga, or breathing exercises can help reduce flare-up triggers and improve overall well-being.
Building a strong support network is a decisive step toward better treatment results and a more positive daily life. You are not alone in this; help is available, and progress is always possible.
When to Consult a Dermatologist?
Recognising when to seek professional care can make a significant difference in treatment success. Early evaluation often improves results and eases anxiety about skin changes.
Consider booking a dermatology appointment if you notice:
- New white patches that appear suddenly or spread quickly.
- Existing patches are increasing in size or number.
- Hair in affected areas is turning white, or similar changes are occurring in other parts of the body.
- Patches develop after physical injury, illness, or high stress.
- Redness, irritation, or inflammation around depigmented skin.
- Emotional distress or loss of confidence due to visible skin changes.
- There is concern about other family members showing similar symptoms.
- Uncertainty about the best sun protection or skincare routine.
Ongoing follow-up visits help track progress and adapt treatment plans when needed. With expert guidance, you can manage the condition safely, effectively, and with confidence.
Conclusion
Managing vitiligo can feel overwhelming at times, but the proper guidance and care make a meaningful difference. Evidence-based vitiligo treatment helps address depigmentation, supports skin health, and provides practical strategies for daily management.
Working closely with a dermatologist ensures you receive personalised care, monitor progress effectively, and adapt treatment plans as needed. Combining medical care with self-care routines and support from family or peer groups strengthens outcomes and helps patients feel confident in their journey.
At Velantis Dermatology, care goes beyond prescriptions. Patients are guided with compassion, evidence-based vitiligo treatment, and ongoing support so they feel heard, understood, and encouraged at every stage of their journey.
Contact Velantis Dermatology to begin your treatment journey with Dr. Janani Sree C M, our trusted MD dermatologist.
FAQ’s
Q1. What is the leading cause of vitiligo?
A1. Vitiligo develops when the immune system mistakenly attacks pigment-producing cells called melanocytes. This disrupts melanin production and leads to white patches on the skin. Genetics, oxidative stress, and other immune-related factors can also contribute to its onset.
Q2. How to increase melanin in skin?
A2. Supporting melanin production involves protecting skin from excessive sun exposure, maintaining a balanced diet rich in antioxidants, and following treatment plans recommended by a dermatologist. Specific medical and light-based therapies can also stimulate melanocytes and encourage re-pigmentation.
Q3. Who is at high risk of vitiligo?
A3. People with a family history of vitiligo or other autoimmune conditions, thyroid disorders, and type 1 diabetes may have an increased risk. High stress, skin injuries, chemical exposure, and early-onset age can also contribute to susceptibility.
Q4. What is the beginning stage of vitiligo?
A4. The initial stage usually presents as small, pale, or white patches of skin. These patches may appear on areas exposed to friction or sunlight and can gradually expand over time if not assessed and monitored.
Q5. How quickly does vitiligo spread?
A5. The speed of vitiligo progression varies among individuals. Some experience gradual changes over several years, while others notice more rapid expansion of patches. Early medical evaluation can help monitor changes and support effective treatment planning.


.png)




