Melasma is a common skin condition marked by dark, irregular patches that often appear on the face, especially in sun-exposed areas. While harmless to physical health, it can affect confidence, emotional well-being, and daily comfort, especially when it becomes persistent or more pronounced over time.
Millions of people worldwide live with melasma, but many struggle with ineffective home remedies or delay professional treatment, allowing the pigmentation to deepen. Early diagnosis and a personalised care plan can make a significant difference in managing melasma and preventing its recurrence.
In this article, we’ll walk you through melasma’s symptoms, causes, and proven treatment options so you can understand your skin better and make informed decisions about its care.
Overview
- What it is: A skin condition causing dark, symmetrical patches, usually on the face.
- Main causes: Hormonal changes, sun exposure, and genetics.
- Symptoms: Brown or grey-brown discolouration, commonly on cheeks, forehead, and upper lip.
- Diagnosis: Physical examination and, if needed, special light or skin tests.
- Treatment: Topical creams, chemical peels, laser therapy, and strict sun protection.
- Long-term care: Consistent skincare, avoiding triggers, and regular dermatologist visits.
What is Melasma?
Melasma is a form of hyperpigmentation in which patches of skin develop a darker colour than the surrounding area due to excess melanin production. These patches typically appear on the cheeks, forehead, upper lip, and nose, and often have a symmetrical pattern on both sides of the face.
The condition is more common in women, particularly during pregnancy or while using hormonal birth control, but it can affect anyone, including men. Melasma is harmless in terms of physical health, but it can be stubborn, recurring, and cosmetically distressing.
While the exact cause isn’t always clear, melasma develops when melanocytes (pigment-producing skin cells) become overactive. This overactivity can be triggered by factors like UV radiation, hormonal changes, and certain skin irritants. Understanding what causes it is essential to managing and preventing flare-ups.
Common Types of Melasma

Dermatologists classify melasma based on the depth of pigment and its distribution pattern. Knowing your type helps in choosing the most effective treatment approach.
- Epidermal Melasma: Affects the skin’s outermost layer and appears as well-defined light to dark brown patches. Often responds well to topical treatments and surface-level procedures.
- Dermal Melasma: Pigment sits deeper in the dermis, creating a bluish or grey-brown tone. Harder to treat and requires more advanced, long-term strategies.
- Mixed Melasma: The most common form, combining epidermal and dermal pigmentation. Shows varying shades of brown and grey, and typically needs a combination approach.
- Centrofacial Pattern: Involves pigmentation on the forehead, cheeks, nose, and upper lip.
- Malar Pattern: Pigmentation mainly on the cheeks and nose.
- Mandibular Pattern: Less common; affects the jawline and lower face, making it harder to detect early.
Now that we’ve covered what melasma is and the different forms it can take, let’s look at the common signs and symptoms.
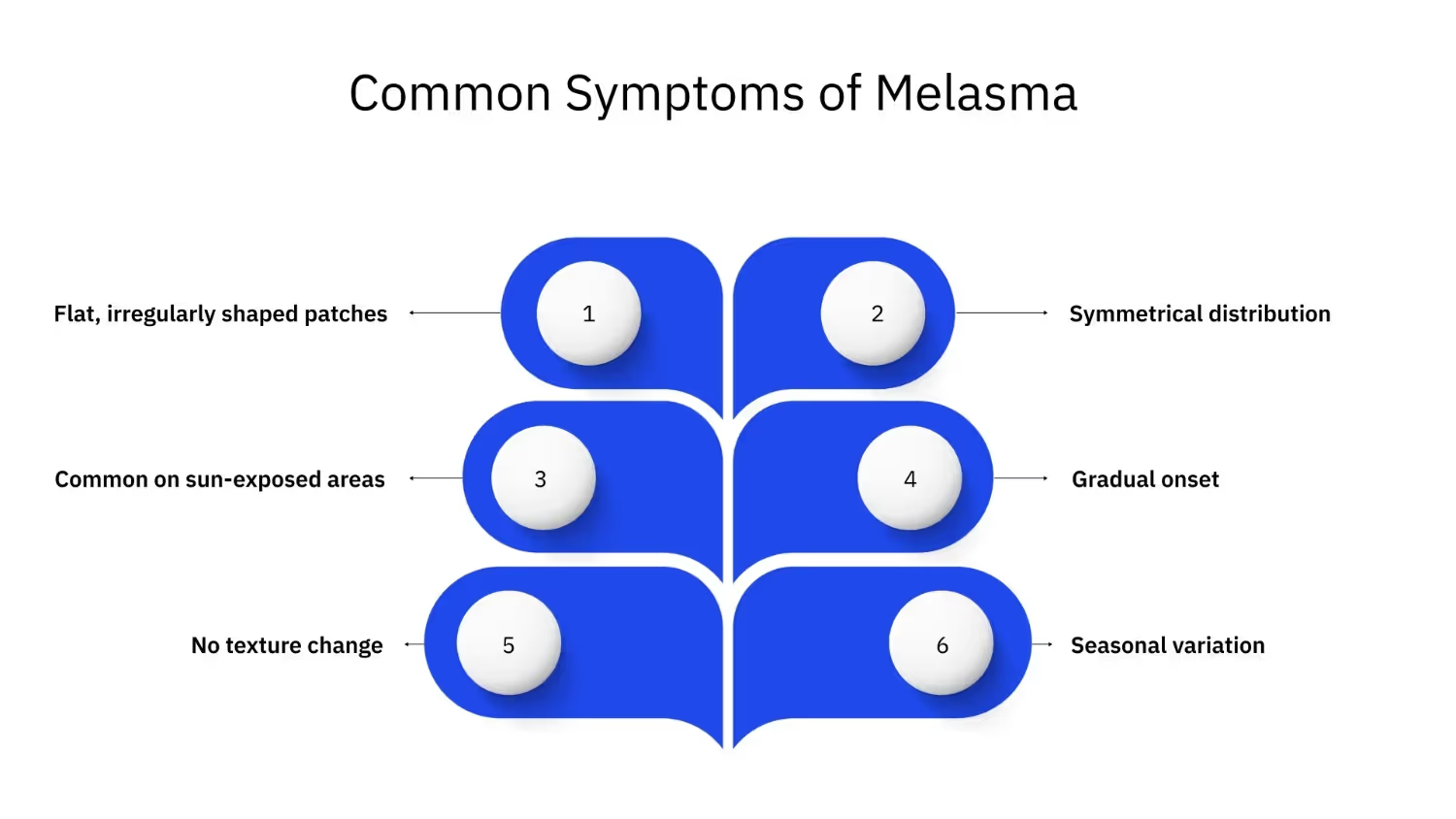
Common Symptoms of Melasma
Melasma is primarily a cosmetic condition and doesn’t cause pain or discomfort. However, its appearance can be distressing for many people. Typical signs include:
- Flat, irregularly shaped patches: Usually light brown, dark brown, or greyish-brown.
- Symmetrical distribution: Patches often mirror each other on both sides of the face.
- Most common on sun-exposed areas: Forehead, cheeks, upper lip, nose, and chin are frequently affected.
- Gradual onset: Patches develop slowly over weeks or months, often worsening with sun exposure.
- No texture change: The skin feels normal; only the colour changes.
- Seasonal variation: Pigmentation may darken during summer and fade slightly in winter.
While melasma’s visible signs are easy to spot, understanding why it develops is more complex.
Common Causes and Triggers of Melasma
Melasma is not caused by a single factor—it’s usually the result of a combination of influences that overstimulate pigment production in the skin. Understanding these triggers can help in both preventing and managing them.
- Hormonal Changes: Shifts in hormone levels, particularly during pregnancy, menopause, or with the use of oral contraceptives, can trigger melasma. This is why melasma is often referred to as “the mask of pregnancy.”
- Sun Exposure: Ultraviolet (UV) rays stimulate melanocytes, the cells responsible for producing pigment. Even minimal sun exposure can worsen melasma, making daily sun protection essential.
- Genetic Predisposition: If melasma runs in your family, you may be more likely to develop it. People with darker skin tones and a family history of pigmentation disorders are at higher risk.
- Certain Medications: Drugs that increase skin sensitivity to sunlight, such as certain antibiotics, anti-seizure medications, or chemotherapy drugs, can contribute to melasma flare-ups.
- Cosmetic Irritants: Harsh skincare products, chemical peels done without proper protection, and fragranced cosmetics can cause skin irritation, which may trigger or worsen melasma in sensitive individuals.
- Thyroid Disorders: Underlying thyroid conditions can influence hormone balance and increase the likelihood of pigmentation issues.
While melasma is often identifiable by its distinct appearance, a thorough diagnosis is essential to confirm the condition, assess the depth of pigmentation, and rule out other skin disorders. This is where a detailed clinical evaluation comes in.
Diagnosis and Assessment of Melasma
Diagnosing melasma is primarily a visual process, but dermatologists often use additional tools to confirm the condition and rule out other pigmentation disorders.
- Physical Examination: A dermatologist will closely inspect the affected skin under good lighting to assess the pattern, depth, and distribution of pigmentation.
- Wood’s Lamp Examination: This handheld light helps determine whether the pigment is located in the epidermis, dermis, or both—information that guides treatment choices.
- Medical History Review: Understanding your hormone status, medication use, family history, and lifestyle habits helps identify potential triggers.
- Dermatoscopy: A magnifying tool may be used to view skin structures and confirm the diagnosis.
- Differential Diagnosis: The doctor may rule out other skin conditions, such as post-inflammatory hyperpigmentation, lentigines, or drug-induced pigmentation, to ensure an accurate treatment.
Once your dermatologist has confirmed a diagnosis of melasma and identified its severity, the next step is to craft a treatment plan tailored to your skin type, triggers, and lifestyle.
Treatment Options for Melasma
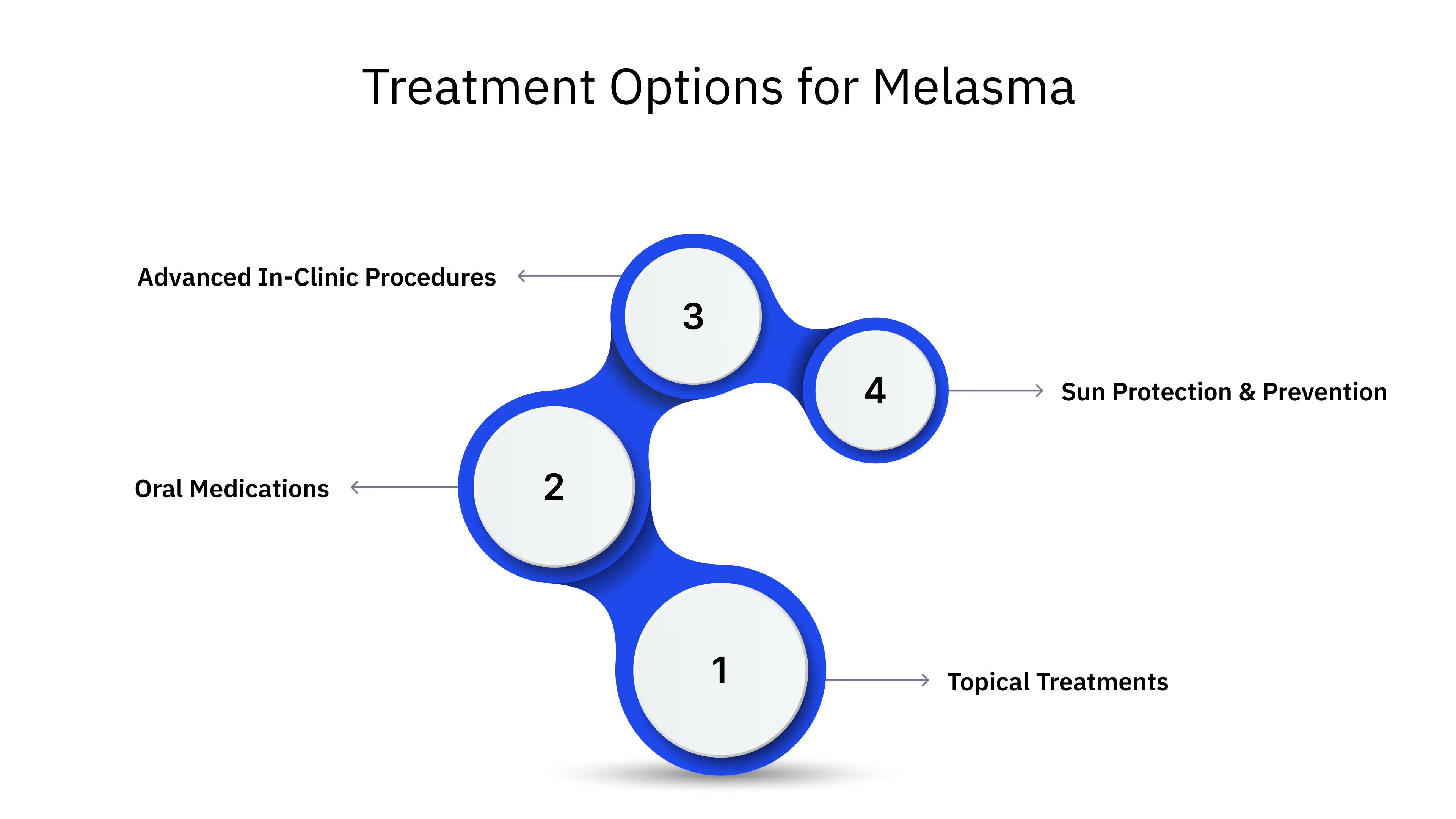
Treating melasma requires a personalised, multi-step approach that focuses on fading existing pigmentation, preventing further darkening, and addressing underlying triggers.
Since melasma can be stubborn and prone to recurrence, dermatologists often combine topical therapies, in-clinic procedures, and lifestyle adjustments to achieve lasting results. Your treatment plan will depend on factors like skin type, severity, and how your skin responds over time, ensuring both safety and effectiveness.
Topical Treatments
These are often the first line of treatment to lighten pigmentation and prevent it from worsening.
- Hydroquinone: A skin-lightening agent that reduces excess melanin production.
- Tretinoin: Promotes cell turnover, helping fade dark patches over time.
- Corticosteroids: Used in combination with creams to reduce inflammation and pigment activity.
- Azelaic Acid: A gentle alternative for sensitive skin, effective in evening skin tone.
- Vitamin C Serums: Antioxidant-rich formulas that brighten skin and protect against free-radical damage.
Oral Medications
In cases where melasma is resistant to topical therapy, certain oral medications may be prescribed under close medical supervision.
- Tranexamic Acid: Reduces melanin production by blocking specific pathways involved in pigmentation.
- Polypodium Leucotomos Extract: A plant-derived supplement that may help reduce UV-induced pigmentation.
Advanced In-Clinic Procedures
Dermatologist-performed treatments offer faster and more noticeable results when topical therapies alone aren’t enough.
- Chemical Peels: Use of glycolic acid, salicylic acid, or lactic acid to exfoliate and fade pigmentation.
- Laser Therapy: Targeted light energy breaks down excess melanin without damaging surrounding skin.
- Microdermabrasion: Gently removes the surface layers of skin, improving texture and reducing the appearance of pigmentation.
- Microneedling with PRP or Serums: Stimulates skin renewal while delivering active ingredients deeper into the skin.
Sun Protection and Prevention
Since melasma often worsens with UV exposure, prevention is as important as treatment.
- Broad-Spectrum Sunscreen (SPF 30 or higher): Used daily, even indoors, to prevent recurrence.
- Physical Barriers: Hats, sunglasses, and clothing to shield skin from UV rays.
- Blue Light Protection: Special sunscreens or skincare products with antioxidants to shield against the light emitted by digital devices.
Struggling with stubborn melasma? At Velantis Dermatology, Dr. Janani Sree C M creates personalised treatment plans tailored to your skin’s unique pigmentation patterns and triggers. Our evidence-based approach combines advanced technology with expert care to help restore a more even, radiant complexion. Book a consultation today and take the first step towards clearer, healthier skin.
Long-Term Management Strategies for Melasma

Melasma often requires ongoing care to prevent recurrence and maintain skin clarity. A consistent approach, both at home and in-clinic, can help you sustain results and protect against triggers.
1. Sun Protection as a Daily Habit
- Use a broad-spectrum sunscreen (SPF 30 or higher) every day, even indoors or on cloudy days.
- Reapply every 2–3 hours when outdoors to ensure continuous coverage.
- Pair sunscreen with physical barriers, such as wide-brimmed hats and UV-protective clothing.
2. Consistent Skincare Routine
- Stick to dermatologist-approved products that are gentle yet effective for pigmentation control.
- Include antioxidants like vitamin C to combat oxidative stress and protect against pigmentation.
- Avoid harsh scrubs or irritants that could inflame skin and worsen pigmentation.
3. Lifestyle and Hormonal Management
- Monitor and manage hormonal triggers—such as pregnancy, contraceptive pills, or hormone therapy—with your doctor’s guidance.
- Maintain a balanced diet rich in antioxidants and anti-inflammatory foods to support skin health.
- Manage stress levels, as chronic stress may influence hormonal balance and pigmentation.
4. Periodic In-Clinic Maintenance
- Schedule follow-up treatments, such as chemical peels, laser touch-ups, or microneedling, as advised by your dermatologist.
- Combine in-clinic sessions with home care for optimal results and longer-lasting improvements.
5. Regular Dermatology Check-Ins
- Have your skin reviewed at regular intervals to catch early signs of recurrence.
- Update your treatment plan based on seasonal changes, lifestyle shifts, or new triggers.
Conclusion
Melasma may be a persistent condition, but it doesn’t have to dictate how you feel about your skin. With a personalised treatment plan, proactive sun protection, and regular dermatologist-guided care, pigmentation can be visibly reduced and effectively controlled. Consistency is key—not just during active treatment but as part of your daily routine—to prevent future flare-ups.
Your skin’s needs can change over time. If you notice new patches of pigmentation or your current plan isn’t working as well, consult your dermatologist promptly. Even small adjustments can make a big difference in preserving a clear and even complexion.
Ready to take control of your melasma? Book your consultation with Velantis Dermatology today and receive a customised care plan tailored by Dr. Janani Sree C M to meet your needs.
FAQs
Q1: Can melasma go away on its own?
A1: In some cases, melasma can fade naturally, especially if triggered by pregnancy or medications that are later discontinued. However, without targeted treatment and sun protection, it may persist or return.
Q2: Is melasma a sign of an underlying health condition?
A2: Melasma is not usually linked to serious illness, but it can be influenced by hormonal changes, certain medications, or thyroid disorders. A dermatologist can help identify and address possible triggers.
Q3: What is the best treatment for melasma?
A3: There’s no one-size-fits-all approach. Treatment often includes topical creams, sun protection, and in-clinic procedures such as chemical peels or laser therapy, tailored to your skin’s specific needs.
Q4: Can sunscreen alone treat melasma?
A4: Sunscreen is essential to prevent melasma from worsening, but it won’t fade existing pigmentation on its own. It should be combined with medical treatments for best results.
Q5: Are there any risks with laser treatment for melasma?
A5: When performed by an experienced dermatologist, laser treatments are generally safe. However, in some cases, they may cause temporary darkening before the improvement is noticeable. Proper patient selection and aftercare are crucial.
Q6: Can home remedies work for melasma?
A6: While some natural ingredients like aloe vera or turmeric may help brighten skin, they are not a substitute for dermatologist-approved treatments and may irritate sensitive skin.
Q7: How long does it take to see results from melasma treatment?
A7: This depends on the severity and chosen treatments. Many patients notice improvement within 8–12 weeks; however, consistent care is necessary for lasting results.
Q8: Does melasma always come back?
A8: Melasma can be chronic and prone to recurrence, especially without strict sun protection. Long-term maintenance is crucial for maintaining pigmentation control.
Q9: What’s the difference between melasma and hyperpigmentation?
A9: Melasma is a specific type of hyperpigmentation often linked to hormonal changes, while hyperpigmentation is a broader term for dark spots from various causes, including acne and injury.
Q10: Is melasma contagious?
A10: No, melasma is not contagious and cannot be spread through contact.


.png)




